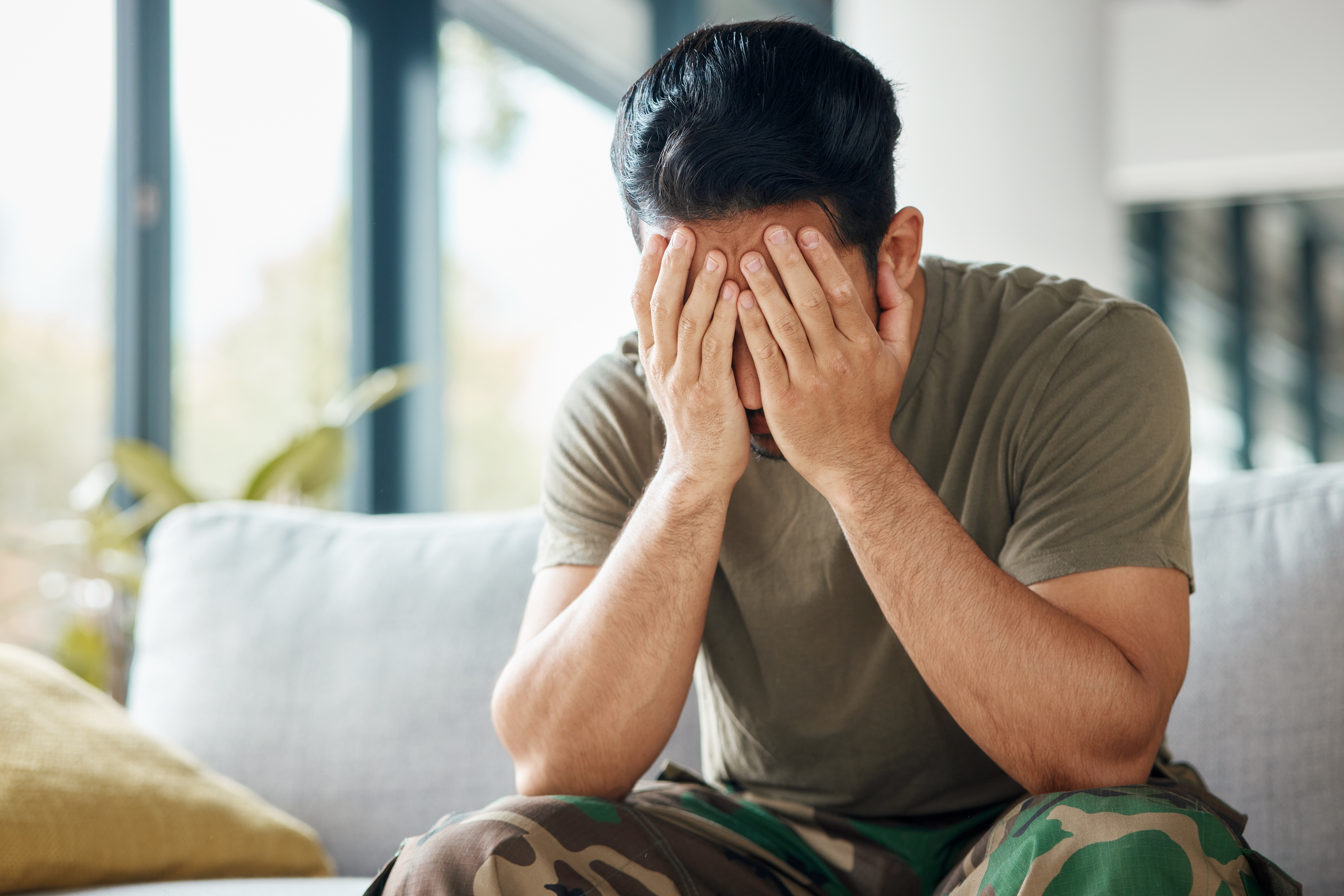
For many military veterans, the scars of battle aren’t just on the outside. Studies show that as many as 30% of veterans develop Post-Traumatic Stress Disorder (PTSD) at some point in their lifetime. To cope, some turn to drugs or alcohol, leading to another battle, this time with addiction. The problem of addiction in veterans is a serious one, as veterans are diagnosed with substance use disorders at a higher rate than the general population. Understanding the connection between PTSD and substance dependence in veterans is important in treating both, as a pattern of use will persist unless the symptoms and triggers are addressed concurrently.
Understanding the Connection between Drug and Alcohol Addiction and PTSD
PTSD is a severe mental health condition that can affect anyone but is seen at significantly higher rates in high-stress professions, such as active-duty military and veterans. It’s characterized by vivid flashbacks, nightmares, and feelings of anxiety, anger, and guilt. Many veterans with PTSD feel they cannot cope with these emotions and often turn to drugs and alcohol to escape. Drug and alcohol addiction is a vicious cycle for veterans with PTSD. The substances help them numb the emotions and memories that come with the condition, but in the long run, it only amplifies the problem. The drugs and alcohol only serve as a temporary escape, and the feelings and memories of the trauma eventually return, creating a cycle of dependence on drugs and alcohol as veterans try to find relief from their pain and distress.
The Impact of PTSD and Substance Abuse on Veterans
The impact of addiction and PTSD on veterans is devastating. Drugs and alcohol only worsen the symptoms of PTSD and make it harder to manage the condition. It can also lead to a host of other problems, including financial difficulties, strained relationships with loved ones, homelessness, and even suicide. “The number one killer of veterans and military is not the enemy. A lot of times, it’s the stigma of reaching out for help is taking more lives, and it’s shown by some of the rates we’ve seen in suicides,” said Jason Smith, CPSS, MSgt USMC (Ret) Veteran’s Business Consultant. In some cases, veterans with PTSD and addiction end up in the criminal justice system, losing benefits and support, making it even harder for them to get the help they need. It’s a vicious cycle that can be difficult to break without proper support and treatment. The impact of the connection also extends to their families and loved ones. The families of veterans with PTSD and addiction often suffer as well, as they struggle to understand and cope with their loved one’s condition. It can be a challenging and lonely experience for them, and they must also get the support they need, such as Al-Anon.
Treating Co-Occurring PTSD and Addiction
The most effective treatment programs use a multidisciplinary approach, blending clinical and medical approaches with peer support to address the complex interplay between trauma and substance abuse and the unique experiences of veterans. In both residential and outpatient rehab settings, addiction treatment programs for veterans often include individual and group counseling, medication, family support, and education to learn to develop healthy coping skills and prevent relapse. Many people who suffer from co-occurring disorders such as PTSD and addiction have also experienced trauma, which can have a profound impact on their lives. Trauma-informed therapy is an approach that recognizes this and adjusts the method of treatment to consider the vulnerabilities and specific needs of the trauma survivor. This therapeutic framework acknowledges the connection between addiction and PTSD and focuses on safety, trustworthiness, choice, collaboration, and empowerment. By recognizing the strengths of the survivor, trauma-informed therapy provides a compassionate therapeutic intervention that can help individuals overcome the impact of trauma and achieve lasting recovery.
Community Support for Veterans in Recovery
“One of the greatest things you can do is provide service to another human being. In our field, when a Vet helps another Vet, we tend to see a better outcome,” said Smith In addition to a qualified treatment program, strong support systems are pivotal in a veteran’s recovery journey. Peer support groups are invaluable, offering a platform for veterans to share experiences and coping strategies with others who empathize with their plight. The consistent involvement of family and friends also serves as a crucial pillar of stability, providing emotional sustenance and motivation. Through professional care, community support, and personal determination, veterans can make significant strides toward reclaiming control over their lives and health.
A Treatment Program Made for Veterans
Bradford at Madison recognizes the unique challenges faced by those who’ve served our country, which is why we’ve created the Hero’s Path Program specifically for veterans and active-duty military struggling with addiction. This program understands that veterans have different experiences and stresses than civilians and need treatment that respects and addresses their needs. Hero’s Path provides a supportive recovery community where veterans can connect with those who truly understand their situation. Bradford’s comprehensive medical and psychological care incorporates evidence-based therapies that are proven to help with addiction, as well as address co-occurring disorders such as PTSD, anxiety, or depression. What’s more, veterans in the Hero’s Path Program can access special services tailored for them, like help transitioning back into civilian life, job search support, and collaboration with other Veterans Administration (VA) healthcare providers.